Roger Sandall
Quadrant, December 2005
The story of Dr Patel
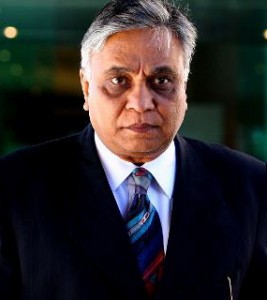 Dr Jayant M. Patel—or ‘Doctor Death’ as he was christened by the Australian anaesthetist who watched his patients die—was first discovered mangling patients fully twenty years ago in New York. Given employment in an Australian hospital in 2003, where he continued on his destructive path, he was until recently the subject of an official governmental inquiry (The Bundaberg Hospital Commission of Inquiry, hereafter “the Inquiry”). This investigation involved a possible total of 87 deaths, and in an interim report of June 10, 2005, the Commissioner recommended that Patel be charged with murder. Prosecution may be difficult, however, for with the active connivance of Queensland health administrators he fled back to America last April, and his present whereabouts are unknown.
Dr Jayant M. Patel—or ‘Doctor Death’ as he was christened by the Australian anaesthetist who watched his patients die—was first discovered mangling patients fully twenty years ago in New York. Given employment in an Australian hospital in 2003, where he continued on his destructive path, he was until recently the subject of an official governmental inquiry (The Bundaberg Hospital Commission of Inquiry, hereafter “the Inquiry”). This investigation involved a possible total of 87 deaths, and in an interim report of June 10, 2005, the Commissioner recommended that Patel be charged with murder. Prosecution may be difficult, however, for with the active connivance of Queensland health administrators he fled back to America last April, and his present whereabouts are unknown.
* * *
Patel was born in 1950 in Jamnagar, Gujarat, India, receiving his qualifications from the M. P. Shah Medical College in his hometown in 1973. While I haven’t visited Jamnagar, I know the region and adjacent towns, and although a qualitative ranking of Indian medical schools is unavailable, I think we may say with some confidence that in 1973 the M. P. Shah Medical College did not rank very high. In 1977 Patel moved to the United States, training as a surgeon in Rochester and Buffalo between 1978 to 1984, meanwhile working as a resident trainee surgeon at a local hospital.
In 1984 New York health officials cited him for failing to properly examine patients before surgery (we find exactly the same thing later in Australia), fined him US$5,000 for negligence, and placed him on three years’ clinical probation. Just as important is the fact that the American report also charged Patel with “moral unfitness to practice” medicine under New York law. According to an article in The Oregonian by Don Colburn and Susan Goldsmith (22.04.05) it accused him of falsifying operating theatre reports, “abandoning or neglecting a patient in need of immediate professional care”, and “harassing, abusing or intimidating patients either physically or verbally”.
In 1989 he moved to Oregon and joined the Kaiser Permanente Hospital as a general surgeon in Portland. How was work at this hospital found so easily? Colburn and Goldsmith show that in 1988, four years after Patel had been disciplined in New York for “negligence, incompetence, and unprofessional conduct”, a prominent Rochester surgeon named J. Raymond Hinshaw (now deceased) wrote the Oregon Board of Medical Examiners that Doctor Death showed “technical and professional brilliance”, and when asked for further detail responded with a strong defence of Patel’s application for a post as surgeon: the proceedings against Patel, he claimed, consisted of the “harassment of a brilliant young surgeon”, a man he would recommend “without reservation.”
Over in Oregon, according to Kathleen Haley, Executive Director of the Oregon Board of Medical Examiners, his glowing New York references carried more weight than his dismissal from the residency program in 1981, or his $5000 fine; and they successfully nullified the New York disciplinary action for negligence, incompetence, and unprofessional conduct. Another spokeswoman for the Oregon BME remembered uncomfortably that although the references were superb, she was aware of reports of deaths from Patel’s operations, “likely resulting from his less than quality surgical skills”.
These “less than quality surgical skills” would soon be displayed again. According to the useful Wikipedia entry it wasn’t long before Patel’s perverse enthusiasm for cutting and stitching human flesh was being noted at the Kaiser Permanente Hospital in Portland too: “Medical staff alleged that he would often turn up, even on his days off, and perform surgery on patients that were not even his responsibility. In some cases this surgery was not even required, and caused serious injuries or death to the patient.”
And yet, amazingly, the state of Oregon allowed him to mutilate, disable and kill a succession of patients over a period of nearly ten years. Eventually however even the Kaiser Permanente Hospital appears to have had enough. In 1998 it reviewed 79 surgical cases by Patel and found the evidence so disturbing that the hospital banned him from operating for pancreatic and liver surgery, required him to seek a second opinion on all complicated cases, and alerted the Oregon Medical Board.
When the Oregon Medical Board conducted its own review of the Kaiser Permanente cases it looked closely at four of them. Three had died, while a fourth lost gastrointestinal function after Patel performed a colostomy backward. The victim (this is the only appropriate word) had gone into surgery to have his colon fixed and ended up with his urethra severed. “They had to rearrange my testicles to take skin off to fix the urethra,” he said in a television interview in June 2005, “and it left me impotent.” Repairing the damage done by Patel took an additional four operations. “It appears in retrospect that he was a sociopath,” the victim added, suggesting that “when he went to Australia he became a psychopath.”
In the same Australian television program Oregon Medical Association associate executive director Jim Kronenburg said he was shocked by the havoc Dr Patel wrought, citing the case of a clamp that was left in the stomach of one patient. “Many of these things are not an issue of competence or judgment – they are just wrong,” he said. “They are things that no physician in my long experience would even contemplate doing. I mean they are just crazy.” Such was the Oregon record of Hinshaw’s “brilliant” applicant for a surgeon’s post in Portland, a man he recommended “without reservation”.
Time was now running out, and when the Oregon Board of Medical Examiners further restricted his permit to practice in September 2000, and with New York State forcing him to surrender his license in April 2001, it was time to jump ship.
The Australian option
But where could Doctor Death go? Where could a man like this find both employment and a salary of the kind he now expected and required, when his record was known in the USA, and when anyone who studied that record would suspect he was not merely incompetent but quite possibly mentally unbalanced—a man with a barely controllable urge to cut and slash, who shouldn’t be allowed within five miles of an operating theater?
For such a person there were I suppose two broad possibilities—South America and Australia. Both are common refuges for rogues and runaways. But in South America malefactors like Patel could easily get a bullet no questions asked: for any number of reasons Australia was a better option. Rumor had it that its citizens were so easy-going that even a 20-year record of medical mayhem might not be noticed, and a conman could easily pull the wool over their eyes. At the same time the Australian media’s eagerness to appease whoever claimed to be the victim of racial prejudice ensured that there should always be sympathisers to conceal his delinquencies and prevent them coming to light.
Anyway, Australia is where Jayant Patel turned up next. He was made a Senior Medical Officer at Bundaberg Base Hospital in April 2003, and later became Director of Surgery. It must not be thought that his application wasn’t vetted—it was. But Patel confidently lied his way through the relevant questions. Asked among other things if his license to practice had ever been subject to suspension or cancellation, he answered no, smoothly signing a declaration to the effect that “the above statements are true and correct.” At the same time the employment agency in Australia that steered Patel toward Bundaberg Hospital received almost a dozen persuasive referees’ letters from America, all dated 2001.
* * *
Before long the mad mangler was at it again. The Bundaberg Base Hospital is not a major facility. On a ranking of 1 to 3 it has only a Level 1 unit for post-operative intensive care. But when Toni Hoffman, a senior nurse who manages the Intensive Care Unit came back from a holiday in June, 2003, she found that “Dr Patel was wanting to do very complex and large-scale surgeries which really didn’t fit within our scope of practice.” He seemed particularly keen to relieve a patient of his oesophagus if he still had one; and when a man arrived in a desperate condition (with virtually inoperable cancer according to the much bigger hospital in Brisbane where he had been first examined, a place with a top-rated ICU designated Level 3) Doctor Death saw his chance.
Bullying his associates into silence, falsifying the theatre records as he went along (the patient was ‘stable’ he wrote, when in fact the patient was brain dead), he cut out the oesophagus of a man who then died six days later. Note that this is still mid-2003, at the start of his Australian career, and that most of the 1,202 patients he treated before fleeing the country were yet to come. But already concern was being expressed by staff at Bundaberg, and already attempts were being made to warn higher levels of the Queensland health bureaucracy. On the one hand a shocked Ms Hoffman in the Bundaberg ICU tried to alert administrators about the situation; on the other, Dr Cook at Brisbane’s Mater Hospital wrote a lengthy critique pointing out how inappropriate it was to perform such operations at Bundaberg. Both warnings were filed and forgotten.
Patel’s character and behavior at this time are well conveyed in the following excerpt from the transcript of Ms Toni Hoffman, (Bundaberg Hospital Commission of Inquiry, Transcript for May 23 2005.)
His whole persona and his whole bravado about things didn’t match up. One day he would say he had trained in the ‘States and had 15 years as a trauma surgeon. The next day he would say he had 25 years as a cardiothoracic surgeon. Every day there was a different qualification… and he was very loud, and very old-fashioned in his views about the drugs and treatments we use nowadays in intensive care.
He was about 20 years behind. Like, we’ve gone full circle in the types of drugs and things that we do in intensive care, and he was way back there, but he would consistently refer to Australia as the “Third World”, and say that by coming over here he was doing us a favor, that he didn’t need the money, and how backward we were in caring for patients… So a whole picture was evolving about Dr Patel.
Right from the start Miss Hoffman raised the alarm about Patel’s criminal carelessness—nicked aortas causing patients to bleed to death, punctured bowels causing fatal infections, oesophegectomies with wounds that never healed, apparently simple injuries like crushed toes that developed into gangrene and after that to amputated legs, along with a notorious indifference to hand-washing hygiene that led nurses to call him Dr E. Coli (“doctors don’t have germs” he said to reassure them). As the Manager of the Intensive Care Unit these cases usually became Hoffman’s responsibility—despite overburdened facilities that could hardly cope—and there they often died.
Right from the start she tried to get the Director of Medical Services, Dr Darren Keating, and the District Manager of the Bundaberg Health Service, Mr Peter Leck, to listen to her concerns. Dr Keating retorted that Patel was “a very experienced surgeon” and implied that they were lucky to have him on staff. Mr Leck repeatedly turned a deaf ear to all appeals. When a new Director of Nursing, Ms Linda Mulligan, was appointed at the hospital, Hoffman tried to enlist her help. But it was soon obvious that Ms Mulligan had no intention of involving herself in the wards. Withdrawing into the comfort of her administrative quarters, she emerged only when it suited her—though she did give Hoffman a book to help the manager of the Intensive Care Unit resolve what she believed was an unjustified personal hostility to Patel. If that failed, she said, then perhaps Hoffman should seek psychological counselling.
Meanwhile the toll of the mutilated and the dead continued to rise as a number of irrational, counter-productive practices were instituted by Bundaberg’s Director of Surgery. He wouldn’t allow any patient out of his busy unwashed hands, however severe the case. In a very Indian way, he seemed to feel that it would diminish his status to admit there was anything he couldn’t do, or anything he didn’t know. If he were to make such an admission he would in a sense “lose caste”. Despite the known limitations of Bundaberg’s facilities, therefore, and despite the basic level of its Intensive Care Unit, he refused to allow patients to be transferred to hospitals in Brisbane better equipped and staffed for handling complicated procedures.
If Hoffman stubbornly pressed to have a patient transferred, Patel responded by threatening to resign, and shouting that his operations were bringing $500,000 per year in revenue to the hospital. As in New York twenty years before, he couldn’t leave anyone’s patient alone, sometimes whisking them into the surgery for unwarranted “operations” without informing the doctor to whom they belonged. After this had happened a few times, with fatal results, the Director of Medicine at the hospital (who has a separate jurisdiction to the Director of Surgery) privately ordered the nursing staff never to allow Patel near his patients, and to watch them night and day; while the nurses themselves began hiding patients from Patel in order to keep them alive.
Surely the theatre records showed what was happening? But these were most unreliable. Habits of deception first seen in New York were continued at Bundaberg. Reports were systematically altered, their language strategically euphemised. The rate of post-operative infection had gone up noticeably after Patel began work at Bundaberg, and wounds that should have healed did not, the sutures failing and the two sides falling apart. This is called “dehiscence”; but Patel forbade the use of the term in reports. Dehiscence, he explained, was something else entirely. Discharge summary forms also had their language edited so that key issues were never picked up. As for “adverse events” forms, staff working close to Patel were too frightened to fill them out. Some flatly refused to; some lost the forms; some said “what’s the point?”
The truth of the matter is that after a year Patel had established what amounted to a reign of terror. The younger surgical staff, men anxiously completing their last years at medical school, were fearful of rocking the boat in any way. Others, some of them also immigrant practitioners, were fearful of being sent home if they caused trouble.
A marginal psychopath?
It has been suggested earlier that there is a psychopathically sadistic streak in Dr Jayant Patel. A number of pointers lead in that direction: the body-snatching syndrome—a perverse and obsessive pursuit of human material for his knife, including patients belonging to his colleagues that his colleagues were desperately trying to hide; the invention of bogus clinical reasons to operate—reasons that competent observers denied existed; and besides this an attitude of callous indifference to his patients after surgery, regardless of their distress and whether or not the operation had succeeded or failed.
The opinion of the US victim of a back-to-front colostomy that left him impotent has already been mentioned in this regard (Patel he said was “a sociopath in Oregon, who became a psychopath in Australia”). In Australia he undertook an operation without anaesthetic. From the evidence presented by Dr Miach, the Director of Medicine at Bundaberg Hospital, who stumbled accidentally upon the scene, a pericardectomy was being performed although the patient “wasn’t properly anaesthetised, he wasn’t anaesthetised at all, and the patient was quite distraught… he was agitated, he was moving, he was sort of moaning, he was screaming. It was quite a procedure.” (Bundaberg Hospital Commission of Inquiry, Transcript for May 26, 2005, page 97/293)
This is bad enough. But the treatment and death of a Mr Bramich places the matter, in my view, beyond doubt. The victim in this case came into the Bundaberg Hospital after being severely crushed by a caravan. For a number of reasons it was appropriate for him to be transferred to the Princess Alexandra Hospital in Brisbane—including the fact that the Brisbane hospital had cardiopulmonary by-pass facilities—and a bed was quickly arranged at that institution.
But as soon as he saw the patient the transfer was blocked by Patel, who promptly took Mr Bramich away from another doctor. According to Doctor Death the injured man’s condition was not serious; and anyway, as he boasted to the distressed family, “I’ve been a cardiothoracic surgeon for 15 to 20 years, and if he needs anything I can do it here.” Indeed, the patient’s problems were so minor, according to Patel, that he thought nothing of interrupting his treatment of Bramich to slip out, cross to the operating theatre, and do a colonoscopy on someone else at the same time—in the course of which he managed to perforate the second patient’s bowel! [Imagine the unwashed hands rushing from the bungled colonoscopy back to deal with the blood now accumulating in Bramich’s chest…]
All senior medical opinion was that Bramich should go to Brisbane as soon as possible. This was vetoed by Patel, who then proceeded (after leaving an anaesthetist to deal with the patient whose bowel he had casually perforated minutes before) to extract blood from around the heart, a procedure called pericardiocentesis. There was no indication that this procedure was required—but here Toni Hoffman’s evidence to the Commission of Inquiry is best presented in her own words. Note that Hoffman was not herself present throughout this episode, which went on into the evening. Her account is that reported to her next day by a nurse who was present, and who was trying to care for Bramich:
We just didn’t know who to go to who would listen to us (Hoffman speaking) and the nurse—one of the primary nurses who was looking after him—describes Dr Patel’s using a stabbing motion…
Dr Patel decided he was going to do a pericardiocentesis, which is to try to get some fluid out from around the heart. He’d done an ultrasound first, and this showed there was no fluid around the heart. There was no indication to do this.
But Dr Patel decided he was going to do it anyhow, and the nurse who was caring for the patient described Dr Patel using a stabbing motion into the man’s heart around fifty times with a hard needle, not the normal type of thing that you use for pericardiocentesis.
Then the patient died. His death was witnessed by his 9-year-old daughter. When the patient’s wife gave way to grief, we are told that Patel screamed at her not to cry. For the nursing staff this episode was past bearing—next morning both Hoffman and the nurse who had been obliged to witness these events resolved to act:
She was so disturbed about this—we all were obviously—we were all of us so disturbed about this man’s care that we all wrote letters, and we called the union. We called our union because we didn’t know what to do and the union started to give us advice about what we could do, and also how to formulate our statements, and they also had their legal people read our statements before we handed them in.
Someone called a “quality control coordinator” provided the nurses with a “sentinel event form” to fill out, and this they duly did, but the Director of Medical Services, Dr Keating, downgraded it to not-so-urgent status. Next Hoffman tried to get the Director of Nursing, Ms Mulligan, to act, but unfortunately Ms Mulligan couldn’t see her for two weeks; and when she did grant her an audience, Ms Mulligan recommended that Nurse Hoffman read a 1970s book about personal conflicts and perhaps seek counselling.
Climax and disclosure
This was in July 2004. The stubborn bureaucratic refusal of Keating, Leck, and Mulligan to do anything whatever about the month-by-month mayhem in their midst—to even recognize there was a problem—continued to the end of the year; but by this time the efforts of Toni Hoffman and other concerned nurses to have Patel investigated were at last beginning to show results. One or two people in Brisbane were listening. It looked as if word about Doctor Death was finally getting out, and that the administrators at the Bundaberg Hospital would have to do something at last.
And indeed they did do something—something as scandalous as their previous inertia. Patel was now officially under investigation. Yet on December 24, as a kind of appreciative Christmas gift, Dr Keating wrote and offered to extend his contract for a further four years. (See Appendix A.) This was the last straw: Hoffman now decided to go outside the health system despite the dangers of doing so. She approached a member of the Queensland state parliament, and there the matter was first raised publicly in question time by the Queensland Shadow Minister of Health on March 22, 2005.
Yet this only strengthened the determination of Dr Keating and Mr Leck to defend and protect the interests of their malignant employee. In a fury, Leck summoned the hospital’s nursing staff and denounced the still unnamed whistle-blower who had taken information to parliament, threatening her with both dismissal and a term in a Queensland gaol. Didn’t she understand the terrible harm she had done? Why, he said, the open and critical public discussion of Patel’s activities that was taking place would “divide the doctors and nurses; stop patients coming to the hospital; and erode community confidence” in the hospital’s affairs. (From Exhibit 4, Ms Hoffman’s statement to the inquiry.)
The subsequent furore forced Patel’s resignation and brought an immediate outpouring of grief and indignation from the families of the dead and injured, along with expressions of political disgust for the Labor government. But even this had no effect on Bundaberg Hospital’s leading bureaucrats. Dr Keating wrote an appreciative letter thanking Patel for “his sustained commitment, ongoing enthusiasm and strong work ethic.” On behalf of the Bundaberg District Health Council the Chairman wrote “to offer our support and to advise that we are deeply saddened and appalled by the disclosure in Parliament.” And acting with indecent haste Mr Leck approved a $3500 international airfare to get Patel safely out of Australia.
How did it happen?
Patel’s disastrous career appears to have been made possible by three powerful forces: (1) The pressures felt by junior doctors fearful of creating difficulties for themselves by trying to oust a superior in the medical system, and perhaps also the existence of a kind of misguided professional loyalty. (2) The bureaucratic procedures and more especially the bureaucratic mentality of state hospital administrators. (3) A disinclination to expose an Indian-born surgeon, however menacing he was to public health, lest this bring cries of “racism” from the usual suspects.
* * *
At Bundaberg Hospital, over a period of two years, there must have been at least a dozen doctors aware of what was taking place. But some were only visitors, some were immigrant doctors who did not want to jeopardise their status, and some were young men with families fearful of the economic consequences of trying to get rid of a powerful and aggressive superior. All of them hoped to solve a problem they mainly saw as endangering their personal careers by moving on. One senior and permanent member of the medical staff, the Director of Medicine Dr Miach, having tried unsuccessfully to alert Keating to the situation, simply “told everybody not to go near him”. He developed “work around” solutions excluding Patel from certain procedures and keeping him out of the loop when cases had to be saved by transfer to another hospital. What is disturbing however is that though it was impossible to deal with Patel internally, within the Bundaberg Hospital system, nobody other than Ms Hoffman was prepared to go public on the issue.
An outside doctor, however, had already raised serious questions back in 2003, at the same time as Ms Hoffman herself, though no more attention seems to have been given to his report than to hers. Dr Peter D. Cook of the Mater Hospital in Brisbane was just as shocked to learn of the fatal oesophagectomy performed by Patel in June 2003 as Hoffman was to see it, and wrote in July to senior administrators in Brisbane questioning (a) Whether the surgeon was adequately trained, and suggesting that the advice of the Royal Australian College of Surgeons be sought. (b) Whether the surgeon had adequate recent experience performing the procedure. (c) Whether Bundaberg Hospital had sufficient backup facilities to allow support of such complex patients. “Clearly”, he wrote, “with a Level 1 Intensive Care Unit this is not the case.” In a letter of July 2003, he reported speaking directly to Dr Keating about the matter. (Bundaberg Hospital Commission of Inquiry, Exhibit 218)
But far more sinister than the inhibitions of the doctors at the Bundaberg Hospital was the immoveable and impenetrable bureaucratic regime run by Dr Keating, Mr Leck, and Ms Mulligan. The mental and organizational world in which such men and women live has been the subject of critical discussion from the birth of modern sociology, and Max Weber’s devastating description of the emerging class of German state bureaucrats—their conceit, arrogance, and presumption—is as relevant today as it was 100 years ago:
Rulers without honor, administrators without heart, priests without conviction, this nullity imagines that it has attained a level of civilisation never before achieved.
It is virtually impossible to describe the ingrained evasiveness, the compulsive buck-passing, the deliberately obfuscatory language, the strategic amnesia, and the mechanical citing of rules to excuse the inexcusable, displayed by the Bundaberg Hospital administrative staff who successfully obstructed Ms Hoffman for two and a half years, and brought death or ruin to hundreds of patients. “Administrators without heart” indeed. How this group of people thought and acted is a frightening example of widespread trends in many government departments today, and is something that has to be seen first-hand to be believed. For that reason I have added Appendices Appendix A, Appendix B, and Appendix C, transcript materials from the Inquiry recording the evidence of Dr Keating, Mr Leck, and Ms Mulligan.
Racism and anti-racism
The evolution of moral terminology is an interesting subject. We have now reached a stage where the charge of “racism” is the most serious charge that can be brought against anyone in public life. Nothing carries more weight, and though legally this is still something of a grey area, socially, professionally, and politically, the consequences of such an accusation are grave indeed. (On the day of writing, a stupid, ignorant, and intoxicated remark by the leader of the Liberal Party in New South Wales has brought his downfall, and possibly the end of his political career.)
This being so, one can see why many of those who knew about Patel’s activities would have been justifiably fearful of speaking up lest their motives be impugned and their careers ruined. The risk of being denounced for racial prejudice would certainly appear to have been an important secondary or unspoken motive for silence and inaction. It is worth noting, for example, that when Toni Hoffman complained about Patel’s out of date methods and long-superseded types of medication, Dr Keating at once told her to remember that “Patel was from another country”. The implication being that it is the duty of all right thinking people to treat other cultural standards with indulgence: evidently, for Dr Keating, that took care of any questions about Patel’s acquaintance with current practice or his competence compared with properly qualified surgeons in the field. Nevertheless one wonders: are all “other countries” equal where medical qualifications are concerned? Should we include Fiji? Would Dr Keating have happily gone under Dr Patel’s knife himself? (See the case of Dr Naidoo et al below.)
In any case, cultural questions are unavoidably bound up with the use of immigrant doctors trained overseas. As an example one might consider the case of another doctor from the subcontinent who became Patel’s loyal adjutant. This young man, who we shall call Dr K, never doubted the skill and knowledge of his master—however dismal the outcomes and however tragic the deaths. Though closely interrogated at the Commission of Inquiry he defended Patel steadily throughout. It was not his role, he implied, either to question or to judge what the great man said. Instead, apparently, it was to respect, follow, admire, and dutifully do what he was told. The picture that emerged from Dr K’s evidence showed not only a disturbing pattern of behavior—but a very Indian pattern too: it is based on the relation of a young disciple to his guru, and not on any concept of moral responsibility, Hippocratic or other (See Transcript at the Inquiry website for July 28, 2005.)
Whether this points to a wider problem involving doctors from the subcontinent is hard to say. It does suggest, however, that small close-knit partnerships in which they work together may develop an ethos sharply at odds with the medical expectations of the modern world. As the Inquiry progressed, a damning report came in from another part of Queensland. Formally commissioned by the Director-General of Queensland Health, and written by two members of the Royal Australian College of Surgeons, it described another highly unsatisfactory situation where orthopaedic surgery by unqualified personnel was taking place. In some respects what was happening bore a close resemblance to the regime of Dr Patel. (Bundaberg Hospital Commission of Inquiry, Exhibit 38).
At Hervey Bay and Maryborough three men provide orthopaedic services together. Their leader is Dr Morgan Naidoo. “Although Dr Naidoo felt that he was somewhat of an expert in the field of total joint arthroplasty,” write joint authors Dr. Peter Giblin and Dr John North in their report to the Director-General, “serious concern was expressed from a number of quarters about Dr Naidoo’s ability to undertake this procedure.”
Dr Naidoo is assisted at Hervey Bay by two other men, Dr Dinesh Sharma and Dr Damodaran Krishna. The report found that Dr Sharma’s “clinical and surgical skills were poor” and recommended that he “not undertake surgical procedures without having a specialist orthopaedic surgeon in the operating theatre at all times.” As regards Dr Krishna, “staff interviews elicited uniformly poor reports” of his performance, and he was described as “lacking basic surgical and clinical skills.”
In each case we find “surgeons” who are over-confident, under-qualified, and seemingly indifferent to the welfare of their patients. Both Dr Sharma and Dr Krishna are graduates of the Fiji School of Medicine and have only superficial supplementary training. Each of them appears to have been recruited by Dr Naidoo, and “although requested, a copy of Dr Krishna’s referees could not be located.” It was reported in the press that because of Dr Naidoo’s frequent absences at his luxury East Brisbane home, his two Fiji-trained offsiders, neither of whom are qualified to perform orthopaedic surgery, “were left to do as they pleased”. That indeed seems to have been the case. All in all, the medical program at Hervey Bay described by Doctors Giblin and North looks seriously bad for your health.
* * *
Appendix A – Dr Darren Keating
Commissioner (Mr Antony J. H. Morris, QC): What is your full name Dr Keating? — Darren William Keating.
And your occupation? — I’m the Director of Services at the Bundaberg Health Service District.
Are you presently acting in that capacity? — Presently I’m on leave with pay.
Right. What is your professional address, is it the Bundaberg Hospital? — It’s care of the Bundaberg Hospital.
Yes. What are your qualifications, Doctor? — I’ve got a medical degree, so I’ve got a Bachelor of Medicine and a Bachelor of Surgery. I have a Masters in Health Service Management and I’m also a Fellow of the Royal Australasian College of Medical Administrators.
In October last year did you receive from Dr Miach a document he described as an audit of the insertion of catheters by Dr Patel? _ Yes, I did.
And did that disclose a 100% failure or complication rate? — It showed, I think, five or six cases of Dr Patel’s, yes, of peritoneal dialysis catheters had not worked.
In your experience, was that a matter of concern? — It was of concern, Commissioner, but there was also no comparators relatively – in time or with other surgeons.
Well, did you ask Dr Miach? — When he handed me the piece of paper, he handed me the piece of paper. I didn’t ask him after that, no.
Did you take any other steps to ascertain whether it was a matter of serious concern? — No, I didn’t.
Was that the only concern brought to your attention by Dr Miach? — As regards?
As regards the clinical competence of Dr Patel? — At the moment, that’s… is what I can recollect, Commissioner.
At about the same time did it come to your attention that Ms Hoffman had been to see the District Manager and raised with him a series of concerns in relation to the conduct of Dr Patel? — Yes, I was made aware of that.
Was a decision made to conduct an investigation into Dr Patel as a result of those matters? — Yes, yes, that’s correct.
Was that decision made at an executive meeting involving yourself, the Director of Nursing and the District Manager? — I recollect that I’d received an email copy of the complaint from Tony Hoffman and that, thereafter, some further hard copies were required by Mr Leck than an investigation – that this needed to be further investigated.
Did you at any time suggest that it was a matter that didn’t warrant investigation because it was simply a personality conflict? — I – I – I – agreed that it needed to – it needed investigation but I was concerned that there was – several aspects to this complaint, including the personality conflict.
* * *
(asterisks mark elision)
Commissioner: On the 24th of December, Christmas Eve of last year, did you offer Dr Patel a further four years of employment? — A – a letter was given to Dr Patel with that information.
And that letter was signed by you? — It was signed by me.
So it’s right to say that on the 24th of December, Christmas Eve, you offered him a further four years of employent? — That is correct.
Why would you be doing that when the man was under investigation? — At that – at that stage there was a number of allegations. I was, at that stage, unaware of the – where that – where Mr Leck was as regards his inquiries with head office.
Did you discus with your District Manager that you were planning to offer him – offer Dr Patel another four years of employment? — he was, he was not aware that that – of that time frame in that letter. That time frame was put in that letter with a view to ensuring that we were able to get sponsorship and a visa for Dr Patel.
I don’t care why it was done. Did you speak to your District Manager before offering a further four years’ employment to a doctor who was then the subject of an investigation? — I spoke to him at – I spoke to him at – a number of occasions about Dr Patel and his ongoing employment.
And did you tell him that you were going to offer Dr Patel another four years’ employment? — That letter of offer was made with a view to – – –
Did you tell him you were going to offer Dr Patel another four years of employment? A very simple question? — Sorry, Commissioner, I don’t recall that I told him about four years.
Is it normal for you to offer extensions of employment to senior medical staff at the hospital without discussing that with the senior District Manager? — It is – I discussed – I said, there was a number of changes I discussed but I didn’t discuss the four-year period with him necessarily but I did discuss ongoing appointments with him as regards the medical staff.
Was it, so far as you were concerned, quite irrelevant that serious issues had been raised by another senior specialist at the hospital regarding Dr Patel’s level of competence? — I did not believe that it was irrelevant, Commissioner, no.
So you were quite happy to have a man on your staff as a senior surgeon who your senior physician regarded as incompetent? — Dr Miach had made me aware of the catheter situation but he had not made me aware of his overall impressions and the measures he’d taken as he described today. (Dr Miach had testified earlier that day.)
In January did you write a letter of, I don’t know how you would describe it, commendation, a sort of gushy letter saying to Dr Patel what a good bloke he was? — I wrote a letter in January. I don’t know exactly what date it is, Commissioner, but I did write a letter in response to a letter from him.
Well, he didn’t ask you for a commendation or a letter of approval or anything of that sort, did he? — He wrote his letter of resignation, saying he would not…
Yes? — He…
What prompted you to write such an effusive letter back to Dr Patel? — At that time – at that time I believed it was a normal response to a letter of resignation.
A normal response when the man resigning is the subject of a pending investigation? — He was – he was the subject of a number of allegations which were to be investigated, amongst the totality of the ICU. In retrospect…
I’m not asking you about retrospect. I’m asking you about at the time? — At the time…
With your knowledge that there were the allegations made by Ms Hoffman, the allegations or the issues raised by Dr Miach, surely it would have been a matter of concern to you? — I was concerned abut, yes, all the issues, including him leaving, and I – I wrote that letter – I wrote that letter.
* * *
Commissioner: It didn’t come to your attention, for example, that nurses were hiding patients from Dr Patel so he couldn’t operate on them? — No.
Didn’t come to your attention again that your senior medical staff were recommending to patients that they seek transfer to Brisbane rather than go under the knife of Dr Patel? — No, Commissioner.
* * *
Commissioner: If the people of Bundaberg were told by your hospital that the man who was wielding the scalpel on them was a surgeon, don’t you think those people were entitled to know that the man wasn’t qualified to be a surgeon under Australian law? — He was registered as a Senior Medical Officer in Surgery.
Well, whether or not you called him a specialist surgeon, don’t you think the people of Bundaberg were entitled to be told before he took the knife to them that this man is not a surgeon by Australian standards or in accordance with Australian law? — He was – yes – if you put it that way, Commissioner, yes, but…
* * *
Commissioner: Could you tell me about the funding system by which the Bundaberg Hospital received extra funding as a result of elective surgery performed by Dr Patel? — I have an understanding of the elective surgery program which included surgery done by Dr Patel and by other surgeons done at the hospital.
Could you explain that program? — It’s an allocation of money by the Minister – by government direction related to the – to the performance of elective surgery with a view to reducing the waiting lists for all elective surgery across the state… There is an incentive scheme which relates to giving you a target of basically a number of patients that get elective surgery and you are funded to achieve that target. If you fail to achieve that target, you do not get all your allocation of funding.
Well, we’ve heard a lot of evidence so far about a procedure called an oesophagectomy. Is that ordinarily classified as elective surgery? — It is
So there was more money coming into Bundaberg Hospital for every oesophagectomy performed by Dr Patel, whether the patient lived or died? — I do not know the exact amount of what they call the waiting for that operation and therefore the amount of funding you would get for an oesophagectomy although it is a complex procedure and are based on… etc.
Appendix B – Mr Peter Leck
Commissioner (Mr Antony J. H. Morris, QC): you knew that Dr Patel wasn’t registered as a surgeon, didn’t you? — No, I didn’t.
I see. No-one told you that? — As – as far as I was aware, he was registered as a surgeon.
I see. And you just didn’t bother to find out? — Well, the responsibility in relation to registration and employment of doctors lies with the Director of Medical Services.
So it was Dr Keating’s fault, was it? — As I indicated earlier, I think Dr Kees Nydam was actually acting as the Director of Medical Services at that time.
Now, Dr Patel’s resignation took effect on the 31st March of this year? — Yes.
And the following day you approved a payment to him in respect of airfares to the United States and accommodation in Brisbane? — Well, I can’t…
Is that right? — I can’t remember the actual process of approval.
Would you have a look at this document and tell me whether it’s your signature on it. Is that signed by you? — Yes.
Thank you. Hand that back. Now, this only took place six weeks ago. You’re not going to suggest this has gone out of your memory are you? — I recall Dr Kees Nydam…
Are you going to suggest it’s gone out of your memory? — I don’t specifically recall signing the document if that’s what you’re asking, but…
You’re not suggesting the signature is a forgery? — No.
So is it your evidence to this inquiry that you might have signed this document but it’s gone completely out of your mind in the last six weeks? — I sign a number of things every day…
I’m sure that’s right. Is it your evidence to this inquiry that having signed this – at the time when this document was generated? — Yes.
Dr Patel was the subject of considerable controversy wasn’t he? — Yes.
He had been named in the state parliament? — Well, there was certainly publicity around him.
Yes. Dr Molloy had gone on television and spoken about him. He was a very controversial man at the time, wasn’t he? — There – there was publicity.
And yet you’re telling us that you can’t remember signing off on a form to approve over $3,500 worth of air travel for him on the 1st of April? — I don’t remember specifically signing it, no.
* * *
All right. Who checked Dr Patel’s contract to ascertain that he was entitled to this three and a half thousand dollars? — I don’t know. I didn’t.
You didn’t. Well, you’ve signed the document as a “Certificate of Authorised Expenditure. Approving Officer: I certify (1) that the charge is one which was necessarily required in the provision of an approved departmental service and is cost justified; (2) that the itinerary was approved by the appropriate senior officer; (3) funds are available and voucher is approved.” Do you realise that you certified those things to the Department of Health? — I authorised the expenditure, yep.
And you certified those things as being true to the Department of Health? — Look…
Do you wish to look at your signature again? — No.
* * *
Commissioner: By April you’d been aware for at least six months of serious concerns about Dr Patel, hadn’t you? — Well, I’d had correspondence from Toni Hoffman in late October 2004.
And that raised very serious concerns about Dr Patel, did it not? — Yes, which were under investigation.
When did that investigation start? — The initial correspondence relating…
No. When did the investigation start? I’m not interested in bureaucratic correspondence going back and forth. When did anyone actually start investigating? — I presume that Gerry Fitzgerald started when he received the correspondence, which would have been around mid-January, and he arrived on site on the 14th of February.
And why did it take from October to mid-January for Dr Fitzgerald to start investigating? — We had been through a process of attempting to identify somebody to conduct the investigation. We’d – there had been several telephone calls. We were then interrupted by the tilt train accident in – on the 16th of November. So, for a period of a few weeks, myself and all of the executive were tied up in doing that…
What! Were you down sort of wrapping the wounds or helping out these patients? — No, there was…
No, I didn’t think so. So why weren’t you able to find someone to conduct this investigation in less than three months? — Because we were busy doing that. Couldn’t find somebody or…
Doing what? — I was talking to Queensland Rail… There was discussions with staff and how they were coping and what they were doing.
Which staff did you discuss how they were coping? — Sorry?
With what staff did you discuss how they were coping? Did you go down to the wards and speak to the nurses and doctors and ask “How are you getting on?” — For a time, over a period of time, I visited night shift and afternoon shift to talk to staff about how they were doing…
What, two trips to the wards?
* * *
Apart from Dr Patel, who was the leading clinician in your hospital at the time? The most senior doctor who was actually seeing patients? — What – what the structure is, we…
No. No, just answer the question. Who was the most senior doctor who was seeing patients? — There isn’t one. There’s like, several.
Okay, there were several. Who were they? — So, we had – if we’re asking for the directors…
Yes. Who were they? — You’ve got the Director of Medicine, Dr Peter Miach.
All right. Did you ask Dr Miach about the concerns raised by Nurse Hoffman? — No.
Why not? — Because that isn’t my role.
I see. It doesn’t worry you that patients might be dying or that 15-year-old boys might be losing their legs. It’s not your role to see whether there might be some truth in these allegations? — It’s the role of the Director of Medical Services in terms of clinical issues. I’m not a clinician.
Appendix C – Ms Linda Mulligan
Mr MacSporran (Counsel for Ms Mulligan): Ms Mulligan, perhaps the simplest way to deal with this is for you to tell us how in your view you showed leadership in this issue.
Ms Mulligan: All right. Once it was identified and I discussed the options with the staff member in question and she didn’t agree to those options and she suggested an alternative we discussed why that would be appropriate. I agreed to the same. I continued, you know, over months chatting to her. She was progressing that matter. When I went to ICU it was evident, and the issue over that patient’s surgery, what it actually was that the issues weren’t resolving. I met with the District Manager and Director of Medical Services and suggested that we try and attempt to have some formal mediation because at this state it was obvious that these two staff members were not able to sort the problem out themselves and Miss Hoffman had not agreed to sitting down the four of us and having a chat about it. I then basically continued along that. There was a discussion obviously with Dr Keating and Dr Patel and we had a plan to go back to Toni Hoffman and offer her again an opportunity to sit down and try and sort these issues out and I believe that that was appropriate and I believe it showed leadership. Obviously, some people have a different view, but I cannot make staff sit down and talk to another staff member if they disagree and if anyone suggests that I do that that can be considered intimidation, I believe.
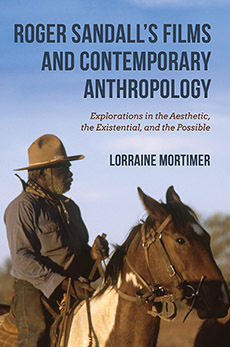
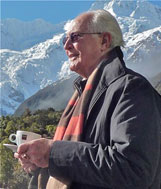 An Australian writer living in Sydney, Roger Sandall is the author of The Culture Cult (2001), a study of romantic primitivism and its effects. His work has appeared in a number of places including Commentary, The American Interest, Encounter, The New Criterion, The American, Sight and Sound, Quadrant, Art International, The New Lugano Review, The Salisbury Review, Merkur, Mankind, Visual Anthropology, and Social Science and Modern Society.
An Australian writer living in Sydney, Roger Sandall is the author of The Culture Cult (2001), a study of romantic primitivism and its effects. His work has appeared in a number of places including Commentary, The American Interest, Encounter, The New Criterion, The American, Sight and Sound, Quadrant, Art International, The New Lugano Review, The Salisbury Review, Merkur, Mankind, Visual Anthropology, and Social Science and Modern Society.